Shedding Light on TBI and PTSD For Brain Injury Awareness Month
March 14, 2024
March marks Brain Injury Awareness Month, a time to highlight two prevalent issues among Service Members and Veterans: Traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD). While both conditions are distinct, they often intersect, profoundly impacting the lives of those who have served in the Armed Forces. Understanding the prevalence, challenges, and avenues for support is vital in fostering awareness and facilitating meaningful change.
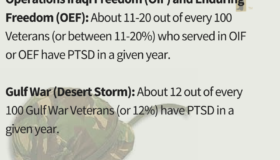
The Prevalence of PTSD in the Military
PTSD is a mental health condition that can develop after experiencing or witnessing a traumatic event. For military personnel, exposure to combat situations, prolonged deployments, and the intensity of their duties significantly elevate the risk of developing PTSD. According to the U.S. Department of Veterans Affairs, approximately 11-20% of Veterans who served in Operations Iraqi Freedom (OIF) and Enduring Freedom (OEF) have PTSD in a given year.
The toll of PTSD extends beyond statistics, affecting individuals, families, and communities. Symptoms may include intrusive memories, flashbacks, hypervigilance, and emotional numbness, significantly impairing one’s quality of life and functioning. Learn more about the warning signs of PTSD here.
The Link Between Brain Injury and PTSD
Traumatic brain injury (TBI) is another prevalent concern among Military personnel, often resulting from exposure to blasts, falls, or other combat-related incidents. The Defense and Veterans Brain Injury Center (DVBIC) reported nearly 414,000 TBIs among U.S. Service Members worldwide between 2000 and late 2019. More than 185,000 Veterans who use VA for their health care have been diagnosed with at least one TBI.
While distinct from PTSD, TBIs can exacerbate symptoms or even contribute to the development of PTSD. The complex interplay between these conditions underscores the importance of comprehensive care and support for Veterans. Research indicates that individuals with a history of TBI may be at increased risk for developing PTSD, as the physical trauma to the brain can impact emotional regulation and cognitive functioning. Conversely, the psychological distress associated with PTSD may hinder recovery from TBI and exacerbate cognitive deficits.
Challenges and Stigma
Despite growing awareness and efforts to destigmatize mental health issues, barriers to seeking help persist within military culture. Concerns about perceived weakness, career implications, and fear of judgment may prevent Service Members from seeking the support they need. Additionally, the invisible nature of these conditions can lead to skepticism or dismissal of symptoms, further isolating those in need of assistance.
The intersection of PTSD and TBI presents unique diagnostic and treatment challenges. Distinguishing between symptoms attributable to each condition and addressing their overlapping effects requires specialized expertise and resources. The good news is that the VA has programs for diagnosing and treating both.
Interesting Fact: Did you know that the prototype for the modern-day CT scan was developed by VA physician and researcher William Oldendorf. He was frustrated by seeing his patients suffer through the medical recommendations at the time for studying brain injury.
Fostering Awareness and Support
Brain Injury Awareness Month serves as an opportunity to advocate for increased understanding, resources, and support for Veterans grappling with these complex challenges. Initiatives aimed at destigmatizing mental health issues, enhancing access to care, and promoting resilience are essential components of comprehensive support systems.
Education and outreach efforts can play a pivotal role in empowering Veterans and their families to recognize the signs of PTSD and TBI, encouraging early intervention and treatment. Peer support networks, counseling services, and community-based programs offer invaluable support and camaraderie to those navigating the journey of recovery.
By raising awareness, fostering dialogue, and advocating for comprehensive support systems, we empower Service Members, Veterans, and their families to recognize the signs of PTSD and TBI, encouraging early intervention and treatment.
PTSD Life-Saving Resources
PTSD can have serious impacts on a person’s life – to include reckless behavior, self-harm, and even suicide. If you or someone you know suffers from PTSD, please share these resources. It could save their (or your) life.
- Chat online with a counselor
- Call 911 or visit a local emergency room
- Dial 988 then PRESS 1 or connect via chat or text (838255) to contact the Veterans Crisis Line. This is a confidential and free hotline for Veterans, Service Members, and their families and friends.
- Veterans in suicidal crisis can go to any health care facility—at VA or in their community—for FREE emergency health care.
- The Veteran Combat Call Center is a 24/7 hotline where you can talk with another combat Veteran: 1-877-WAR-VETS (1-800-927-8387).
- The National Suicide Prevention Lifeline: 1-800-273-TALK